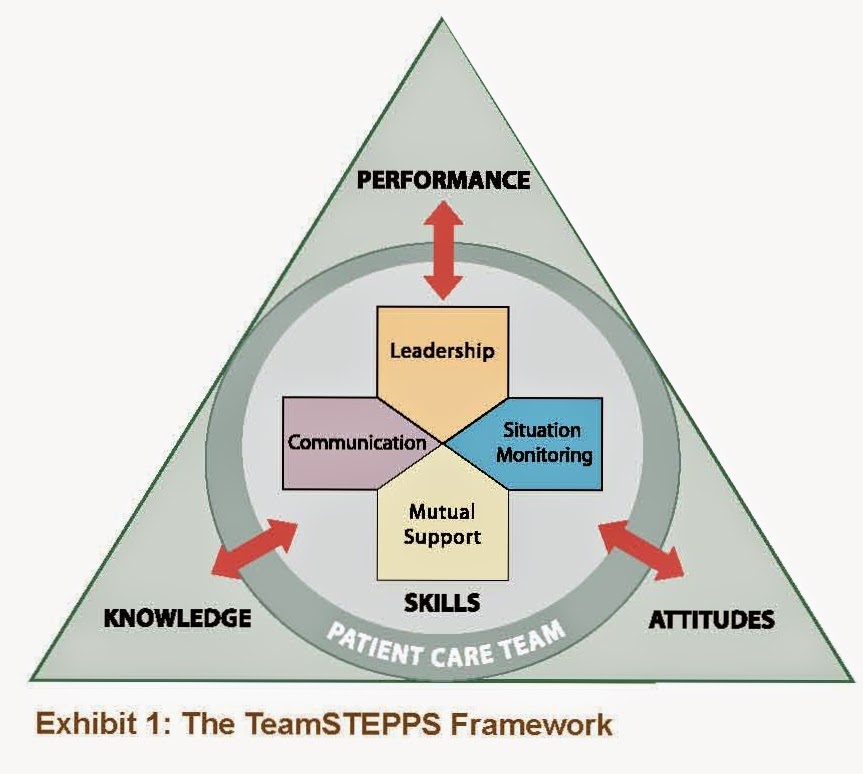
On Improving Medication Safety...

Even though much has been written and spoken about quality healthcare, most of us are pressed to define what it is and how to measure it. The Institute of Medicine (IOM) defines quality healthcare as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.” 1 In the clinical realm, quality healthcare is comprised of six dimensions: Patient safety. Freedom from injury due to medical care and protecting patients from harm. Effectiveness. Efficient care is evidence-based. Patient-centered. The patient is the most important member of the healthcare relationship. We must continually ask: Is care delivered in a patient-centered fashion? Does the system place the patient at the center of every equation in designing the delivery of care? What does the patient value as we evaluate processes and outcomes of care? Involving patients and educating them about the dynamic nature